Intermittent fasting, a dietary approach that cycles between periods of eating and fasting, has gained immense popularity in the health and fitness community.
It involves various methods, such as the 16/8 method (16 hours of fasting and an 8-hour eating window) and the 5:2 method (eating normally for five days and restricting calorie intake for two non-consecutive days).
Many proponents of intermittent fasting claim that it offers numerous health benefits, including weight loss, improved metabolism, and better blood sugar control.
However, as with any trendy diet, concerns and myths have arisen about the potential health risks of intermittent fasting. One of the prevalent worries is whether intermittent fasting could be linked to the development of ulcers.
Ulcers are open sores that can occur in the stomach lining (gastric ulcers) or the first part of the small intestine (duodenal ulcers). They are often attributed to factors like a bacterial infection or the prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs).
In this article, we will explore the existing scientific evidence to determine if there is a credible connection between intermittent fasting and the development of ulcers to answer the question, “Does Fasting Cause Ulcers?”
Understanding Intermittent Fasting

Intermittent fasting, as mentioned earlier, is a dietary pattern involving alternating eating and fasting periods. The 16/8 and 5:2 methods are the most popular approaches, but others exist. During fasting, individuals consume little to no calories, and the eating window allows them to finish their daily caloric needs.
The popularity of intermittent fasting has surged due to claims of its potential health benefits. Proponents argue intermittent fasting may promote weight loss by reducing calorie intake, improving insulin sensitivity, and increasing metabolism.
Additionally, some studies suggest intermittent fasting could positively affect cellular repair processes and reduce inflammation.
As a result, more people have become interested in adopting intermittent fasting as a lifestyle choice. Its appeal lies in its relative simplicity compared to traditional calorie-restricted diets, as it does not dictate specific food choices and can be more flexible to individual preferences.
In the subsequent sections, we will investigate whether intermittent fasting can cause ulcers and examine scientific research on this topic. By doing so, we hope to clarify whether individuals should have legitimate concerns about the potential risk of ulcers while practicing intermittent fasting.
Ulcers: Causes and Risk Factors
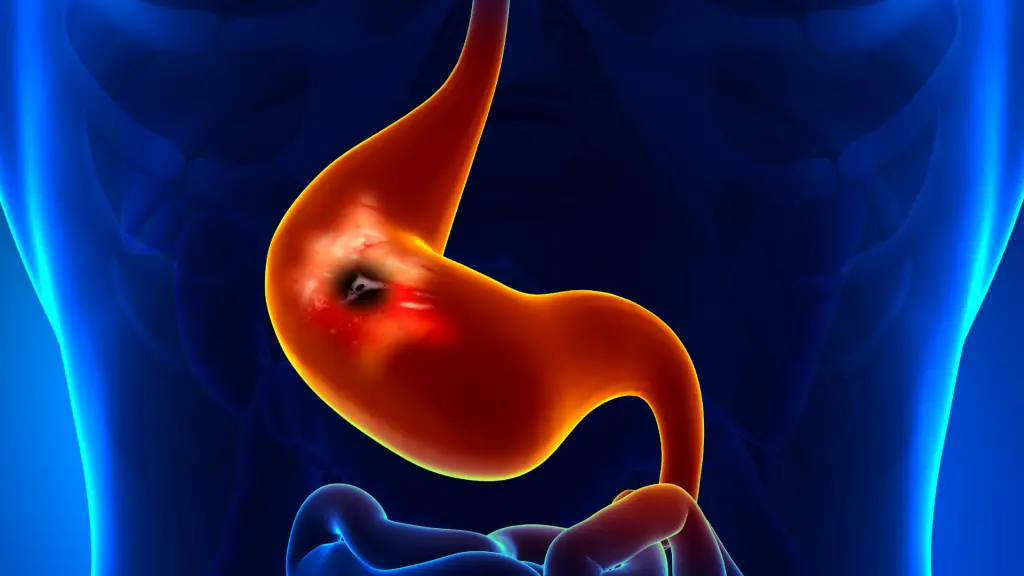
Peptic ulcers are open sores that develop on the stomach’s inner lining (gastric ulcers) or the first part of the small intestine (duodenal ulcers). These ulcers can be painful and may cause discomfort, mainly when the stomach is empty or at night.
The primary cause of peptic ulcers is the erosion of the protective mucus lining that typically shields the stomach and small intestine from the corrosive effects of stomach acid. When this protective barrier is compromised, stomach acid can damage the underlying tissues, forming ulcers.
- H. pylori Infection: Helicobacter pylori (H. pylori) is a bacterium that can colonize the stomach lining and weaken the protective mucus barrier. This makes the stomach more susceptible to acid damage, leading to ulcers. H. pylori infection is a significant risk factor for peptic ulcers and is one of the most common causes.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Frequent or prolonged use of NSAIDs, such as aspirin, ibuprofen, and naproxen, can irritate the stomach lining and increase the risk of peptic ulcers. NSAIDs inhibit the production of prostaglandins, which protect the stomach lining, thus leaving it vulnerable to acid-related damage.
- Excessive Acid Production: Some individuals naturally produce more stomach acid than others, increasing their susceptibility to ulcer formation.
- Stress: While stress alone may not directly cause ulcers, it can exacerbate existing ulcers or delay their healing process. Chronic stress can lead to unhealthy coping mechanisms, such as excessive alcohol consumption or smoking, further developing ulcers.
- Smoking: Smoking is associated with an increased risk of developing peptic ulcers and can hinder the healing process for existing ulcers.
- Alcohol Consumption: Heavy alcohol consumption can irritate the stomach lining and contribute to the development of ulcers, especially when combined with other risk factors like H. pylori infection or NSAID use.
- Maintaining a healthy lifestyle and diet is crucial for reducing the risk of peptic ulcers. Here are some essential steps individuals can take to promote ulcer prevention:
- Avoiding or Limiting NSAIDs: If possible, choose alternative pain relief methods and limit NSAIDs to reduce the risk of ulcer development.
- Managing Stress: Adopt stress management techniques, such as meditation, yoga, or regular exercise, to reduce the impact of stress on the digestive system.
- Treating H. pylori Infection: If diagnosed with an H. pylori infection, seek appropriate medical treatment, usually a combination of antibiotics and acid-suppressing medications, to eradicate the bacteria and promote ulcer healing.
- Quitting Smoking: Smoking cessation benefits ulcer prevention and overall health and well-being.
- Moderating Alcohol Consumption: Limit alcohol intake to moderate levels or avoid it altogether if you have a history of ulcers or are at high risk.
- Eating a Balanced Diet: Consume a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. A balanced diet provides essential nutrients that support a healthy digestive system and may aid in ulcer prevention.
By understanding the common causes and risk factors associated with peptic ulcers and adopting a healthy lifestyle, individuals can take proactive measures to reduce their likelihood of developing ulcers and promote overall gastrointestinal health.
It is essential to note that while intermittent fasting has gained popularity as a dietary approach, addressing and managing ulcer risk factors should remain a priority for anyone considering or currently practicing intermittent fasting.
How Intermittent Fasting Affects Digestion

The digestive process is a complex series of physiological events that enable the body to break down food, absorb nutrients, and eliminate waste. When we eat, the process begins in the mouth, where enzymes break down carbohydrates.
Food then travels to the stomach, where gastric acid and digestive enzymes work together to break down proteins and fats. The partially digested food moves into the small intestine, where further digestion occurs, and nutrients are absorbed into the bloodstream. The remaining waste products continue into the large intestine, where water is absorbed, and feces are formed before elimination.
Intermittent fasting, as a dietary pattern, involves extended periods of fasting interspersed with specific eating windows. During fasting, the body exhausts its readily available glucose stores and begins breaking down stored fats for energy. As fasting progresses, ketone bodies are produced as an alternative fuel source for the brain and other organs.
The fasting period may influence the digestive process by allowing the gastrointestinal (GI) tract to rest without food intake. This rest period could potentially promote tissue repair and optimize digestive functions. However, proponents and skeptics of intermittent fasting have different views on the impact of prolonged fasting on the digestive system.
Numerous scientific studies have investigated the effects of intermittent fasting on the digestive system. Some animal studies have suggested that intermittent fasting can positively affect gut health, such as improving gut barrier function and microbiota diversity. These findings have led researchers to explore whether similar benefits might occur in humans.
In human studies, intermittent fasting has been associated with various digestive changes. Some research indicates that fasting may lead to alterations in gut hormone secretion, which can affect hunger and satiety cues. Additionally, fasting periods may influence gut microbiota composition, potentially impacting overall gut health. However, it is essential to recognize that individual responses to intermittent fasting can vary, and more research is needed to fully understand its specific effects on the human digestive system.
Gastric acid plays a vital role in the digestive process, as it helps break down food and acts as a defense mechanism against pathogens. However, an imbalance between protective factors (mucus lining, blood flow) and aggressive factors (gastric acid) can lead to ulcer formation.
During fasting periods, some proponents suggest that there may be a reduction in gastric acid secretion, which could potentially reduce the risk of acid-related disorders, including ulcers. The logic behind this claim is that less food intake means less stimulation for acid production. However, the human body has sophisticated mechanisms to regulate acid production, and intermittent fasting alone is unlikely to cause significant alterations in acid levels.
While intermittent fasting may cause temporary fluctuations in gastric acid secretion, there is limited evidence to suggest that it has a significant long-term impact on acid production or ulcer formation. Ulcer development is influenced by various factors, including H. pylori infection, NSAID use, stress, and lifestyle choices, and intermittent fasting alone may not be the sole determinant of ulcer risk.
As we continue to explore the potential connection between intermittent fasting and ulcers, it is crucial to consider the broader context and the cumulative effects of various factors on digestive health. Understanding the available scientific evidence will help us draw informed conclusions regarding the relationship between intermittent fasting and ulcer development.
Is Intermittent Fasting Linked to Ulcers?

It is essential to review the existing scientific literature to determine whether there is a credible link between intermittent fasting and ulcer development. Several studies have investigated the effects of intermittent fasting on various aspects of health, including digestion and gastrointestinal health.
A comprehensive review published in the “World Journal of Gastroenterology” analyzed multiple studies on intermittent fasting and its impact on gastrointestinal disorders. The review concluded that no substantial evidence supports a direct association between intermittent fasting and the development of peptic ulcers.
In a randomized clinical trial conducted with individuals practicing Ramadan fasting, researchers evaluated the effects of fasting on gastric health. The study found that contrary to expectations, fasting during Ramadan did not lead to an increased risk of peptic ulcers. The researchers observed no significant changes in gastric acidity or ulcer occurrence among the participants during fasting.
Another study investigated the effects of alternate-day fasting, a type of intermittent fasting, on gastrointestinal symptoms. The research found that participants in the alternate-day fasting group did not experience an elevated risk of gastrointestinal issues, including ulcers. In fact, some participants reported improvements in indigestion and acid reflux symptoms.
Furthermore, a large-scale population-based study published in the “American Journal of Gastroenterology” analyzed data from over 77,000 participants and found no significant association between intermittent fasting and an increased risk of ulcers or other gastrointestinal disorders. The researchers concluded that intermittent fasting did not substantially threaten digestive health.
Despite lacking scientific evidence supporting a direct link between intermittent fasting and ulcer development, some misconceptions and anecdotal claims continue circulating. One such misconception is that intermittent fasting may increase stomach acid production, raising the risk of ulcers. As mentioned earlier, the human body has sophisticated mechanisms to regulate acid production, and intermittent fasting alone is unlikely to cause significant alterations in acid levels.
It is crucial to differentiate between personal experiences and scientific evidence. While some individuals may report gastrointestinal discomfort during intermittent fasting, it is essential to remember that individual responses to fasting can vary widely. Such experiences should not be generalized to imply a direct causal relationship between intermittent fasting and ulcers.
The scientific literature and research studies do not support the notion that intermittent fasting causes ulcers. However, it is essential to approach intermittent fasting or any dietary regimen with a mindful and balanced approach, considering individual health conditions and seeking professional guidance.
As we conclude our exploration, it becomes evident that the available scientific evidence does not indicate a substantial link between intermittent fasting and ulcer development. Nevertheless, personal health considerations and individual responses to fasting should be considered when considering dietary changes or fasting practices.
As the scientific community continues to research the effects of intermittent fasting on various aspects of health, it is essential to remain open to new findings and ensure that decisions about dietary practices are based on evidence-based information.
Potential Risks and Concerns

Intermittent fasting may affect individuals with certain health conditions differently. People with diabetes, eating disorders, or a history of gastrointestinal issues should exercise caution when considering intermittent fasting. The fasting periods and altered eating patterns may impact blood sugar levels, exacerbate eating disorder behaviors, or cause discomfort for those with sensitive digestive systems.
Moderation is key when adopting intermittent fasting. Fasting practices should be tailored to individual needs and lifestyles. Extreme or prolonged fasting without proper monitoring may lead to nutrient deficiencies, fatigue, or other adverse effects on overall health. Listening to one’s body and adjusting fasting routines is essential.
Before starting any fasting regimen, seeking advice from a healthcare professional is crucial, especially if an individual has pre-existing health conditions or concerns about ulcer risk. A medical expert can provide personalized guidance, assess potential risks, and recommend safe fasting practices that align with an individual’s health status.
Balanced Approaches: Intermittent Fasting and Ulcer Prevention

For those interested in trying intermittent fasting while considering ulcer risk, a safe approach is the 16/8 method, which involves an 8-hour eating window and a 16-hour fasting period. This method allows for consistent and sufficient nutrition during the feeding window, reducing the risk of stomach acid fluctuations that could affect ulcer development.
It is crucial to emphasize the importance of consulting a healthcare professional before beginning any fasting regimen, particularly for individuals with a history of ulcers or related health issues. A medical assessment can help identify potential risks and ensure that intermittent fasting is appropriate for an individual’s specific circumstances.
To mitigate potential risks during intermittent fasting, individuals should prioritize hydration, consume nutrient-dense foods during eating windows, and avoid excessive alcohol and caffeine intake. Additionally, practicing stress-reducing activities can further support digestive health and overall well-being. Monitoring any changes in symptoms or discomfort during fasting is essential, and adjustments should be made, if necessary, with guidance from a healthcare professional.
Remember, intermittent fasting should be approached with care and consideration for individual health needs. While the available evidence does not indicate a direct link between intermittent fasting and ulcer development, it is essential to prioritize overall health and well-being when adopting any dietary practice.
Conclusion
In conclusion, the scientific evidence does not support the idea that intermittent fasting causes ulcers. Peptic ulcers are primarily attributed to factors like H. pylori infection, NSAID use, stress, smoking, and alcohol consumption, rather than intermittent fasting alone.
Numerous studies have found no significant association between intermittent fasting and ulcer development. Moreover, intermittent fasting may even offer potential benefits for gut health.
However, it is crucial to approach intermittent fasting with moderation and consider individual health conditions. Consulting a healthcare professional before starting any fasting regimen is essential, especially for individuals with pre-existing health conditions or concerns about ulcer risk.
In summary, intermittent fasting, when practiced responsibly and with consideration for individual health needs, can be safely integrated into a balanced and healthy lifestyle without causing ulcers.
